Introduction: Antigens of the ABO blood group system have an impact on the hemostatic balance. The association of blood group non-O and thrombosis risk is well known. In patients with different bleeding manifestations, an overrepresentation of blood group O has been previously reported (Dentali et al, Semin.Thromb. Hemost, 2013). Nevertheless, the independent effect of the ABO blood group on bleeding severity, when considering VWF as a major contributing factor, has not yet been thoroughly investigated. Patients with bleeding of unknown cause (BUC) have a similar bleeding phenotype as patients with a diagnosis of an established bleeding disorder, but the causes underlying their bleeding tendency are currently unclear and might be multifactorial (Gebhart et al, Haemophilia, 2018). Thus, we investigated the prevalence of blood group O and its role as an independent risk factor for increased bleeding severity in a thoroughly characterized cohort of patients with BUC.
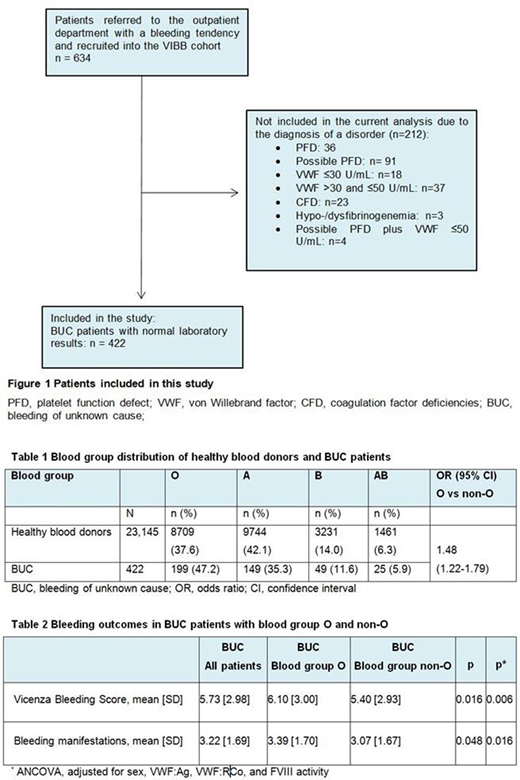
Methods: For this analysis, we selected all patients with normal results in the assessments of plasmatic coagulation and platelet function consecutively recruited between October 2009 and April 2019 within the Vienna bleeding biobank study (Figure 1; Gebhart et al, Haemophilia, 2018). After informed consent, all patients underwent a structured interview on their previous medical and bleeding history including the assessment of the bleeding severity with the Vicenza bleeding assessment tool (BAT). Biomaterial was processed and stored according to standard operating procedures at the Biobank facility (http://www.biobank.at/). A thorough hemostatic laboratory assessment and measurements of thrombin generation, plasma clot properties, and rotational thromboelastometry (ROTEM), as well as platelet function tests (PFA-100, light transmission aggregometry) were performed.
Data on the blood group distribution of 23,145 healthy first-time blood donors were provided by the Austrian Red Cross for comparison.
Results: We observed an overrepresentation of blood group O in 199 out of 422 BUC patients (47.2%) compared to 8709 out of 23,145 healthy blood donors (37.6%), odds ratio for blood group O 1.48; 95% CI=1.22-1.79, p<0.001 (Table 1). Blood group O in comparison to non-blood group O was independently associated with an increased bleeding severity (least square mean [95% CI]: 6.2 [5.8-6.6] vs. 5.3 [4.9-5.7], p=0.006) and a higher number of bleeding symptoms (least square (LS) mean [95% CI] 3.5 [3.2-3.7] vs. 3.0 [2.8-3.2], p=0.016), after adjustment for sex, VWF:Ag, VWF:RCo and FVIII activity (Table 2).
The prevalence of oral mucosal bleeding was significantly higher in blood group O than in patients with a non-O blood group (26.1% vs. 14.3%), even after adjustment for sex, VWF and FVIII, and multiple testing (p=0.013).
When analyzing the influence of blood group O on tests of global hemostatic capacity, results indicated increased clot firmness and reduced lysis in blood group O patients. In ROTEM, the maximum clot firmness was higher (LS mean [95% CI]: 57.4 [56.5-58.3] vs. 55.8 [55.0-56.6] mm, p<0.05) and the maximal lysis lower (LS mean [95% CI]: 13.3 [12.5-14.1] vs. 15.1 [14.4-15.9] %, p<0.05) in patients with blood group O compared to non-O patients, after adjustment for sex, VWF and FVIII, and correction for multiple testing. Also in the analysis of plasma clot properties, the maximum clot absorbance was increased in patients with blood group O after adjustment for sex, VWF and FVIII (LS mean [95% CI]: 0.77 [0.74-0.79] vs 0.71 [0.69-0.74] OD, p<0.05), whereas there was no difference in plasma clot lysis. There was no difference in thrombin generation between BUC patients with blood group O and non-O.
We could not identify any differences in platelet function, as assessed by the platelet function analyser-100 and light transmission aggregometry between patients with blood group O in comparison to non-O patients after adjustment for sex, VWF and FVIII, and correction for multiple testing.
Conclusion: Blood group O is a risk factor for a more severe bleeding phenotype, especially oral mucosal bleeding, independent of VWF and FVIII levels in patients with BUC. Alterations in global hemostatic capacity in BUC patients with blood group O were identified, whereas platelet function was not different. Our data are important for a better understanding of underlying mechanisms of bleeding in BUC patients, which are most probably multifactorial.
Jilma:True North Therapeutics: Consultancy, Other: reimbursement for travel costs for scientific presentations; Bioverativ: Consultancy, Other: reimbursement for travel costs for scientific presentations.
Author notes
Asterisk with author names denotes non-ASH members.